I. Genetic Factors
PCOS is associated with autosomal dominant inheritance, X-linked (sex-linked) inheritance, or gene mutations. Most patients exhibit a normal 46,XX karyotype, while others may display chromosomal aberrations or mosaicism, such as 46,XX/45,XO; 46,XX/46,XXq; or 46,XXq.
II. The Adrenal Androgen Hypothesis
Chom (1973) proposed that PCOS may originate from prepubertal adrenal dysfunction. During intense stress, the adrenal zona reticularis secretes excessive androgens, which are peripherally converted to estrone (E1). This disrupts the hypothalamic-pituitary (HP) axis, causing GnRH-GnH release irregularities, elevated LH/FSH ratios, and increased ovarian androgen production. The resulting hyperandrogenemia leads to ovarian fibrosis, follicular arrest, cystic ovarian enlargement, and chronic anovulation.
(I) Etiology
The exact cause of PCOS remains unclear. It is linked to dysfunction of the hypothalamic-pituitary-ovarian (HPO) axis, adrenal disorders, genetics, and metabolic abnormalities. Some PCOS patients exhibit sex chromosome or autosomal abnormalities, and familial clustering is observed. Recent studies implicate specific genes (e.g., CYP11A, insulin gene VNTR) in PCOS development, underscoring genetic contributions.
(II) Pathogenesis
Key mechanisms include:
- Abnormal Gonadotropin Secretion: Elevated LH with normal/low FSH (LH/FSH ≥2–3), often due to hypothalamic-pituitary dysregulation or disrupted estrogen feedback. Non-cyclic estrone (E1) from peripheral tissues inhibits FSH and stimulates LH, promoting ovarian androgen production and follicular atresia.
- Hyperandrogenism: Excess androgens (testosterone, androstenedione) arise from ovarian or adrenal sources. Ovarian theca cell hyperplasia driven by high LH pulses and enzymatic defects (e.g., aromatase deficiency) exacerbate androgen synthesis.
- Elevated Estrone (E1): Peripheral conversion of androgens to E1, especially in adipose tissue, creates a hyperestrogenic state. This disrupts HPO feedback, perpetuating anovulation.
- Cytochrome P450C17A Dysregulation: Overactivity of this enzyme in ovarian/adrenal tissues increases 17-hydroxyprogesterone (17-OHP) and androgen production. Insulin/IGF-1 signaling further amplifies P450C17A activity.
- Insulin Resistance & Hyperinsulinemia: Present in most PCOS patients, insulin resistance enhances ovarian androgen synthesis and reduces SHBG, elevating free testosterone. Insulin receptor serine phosphorylation defects and VNTR polymorphisms are implicated.
- Obesity: Central obesity exacerbates insulin resistance and hyperandrogenism. Adipose tissue aromatization of androgens to estrogens creates a vicious cycle. Leptin-NPY axis dysfunction may also contribute to LH hypersecretion.
- Hyperprolactinemia: Mildly elevated prolactin (10–15% of cases) may stem from estrogen excess or dopaminergic deficiency. Bromocriptine (a dopamine agonist) can improve symptoms.
- Autoimmunity: Controversial role; some studies suggest anti-ovarian antibodies or lymphocytic infiltration in follicles, but evidence remains inconsistent.
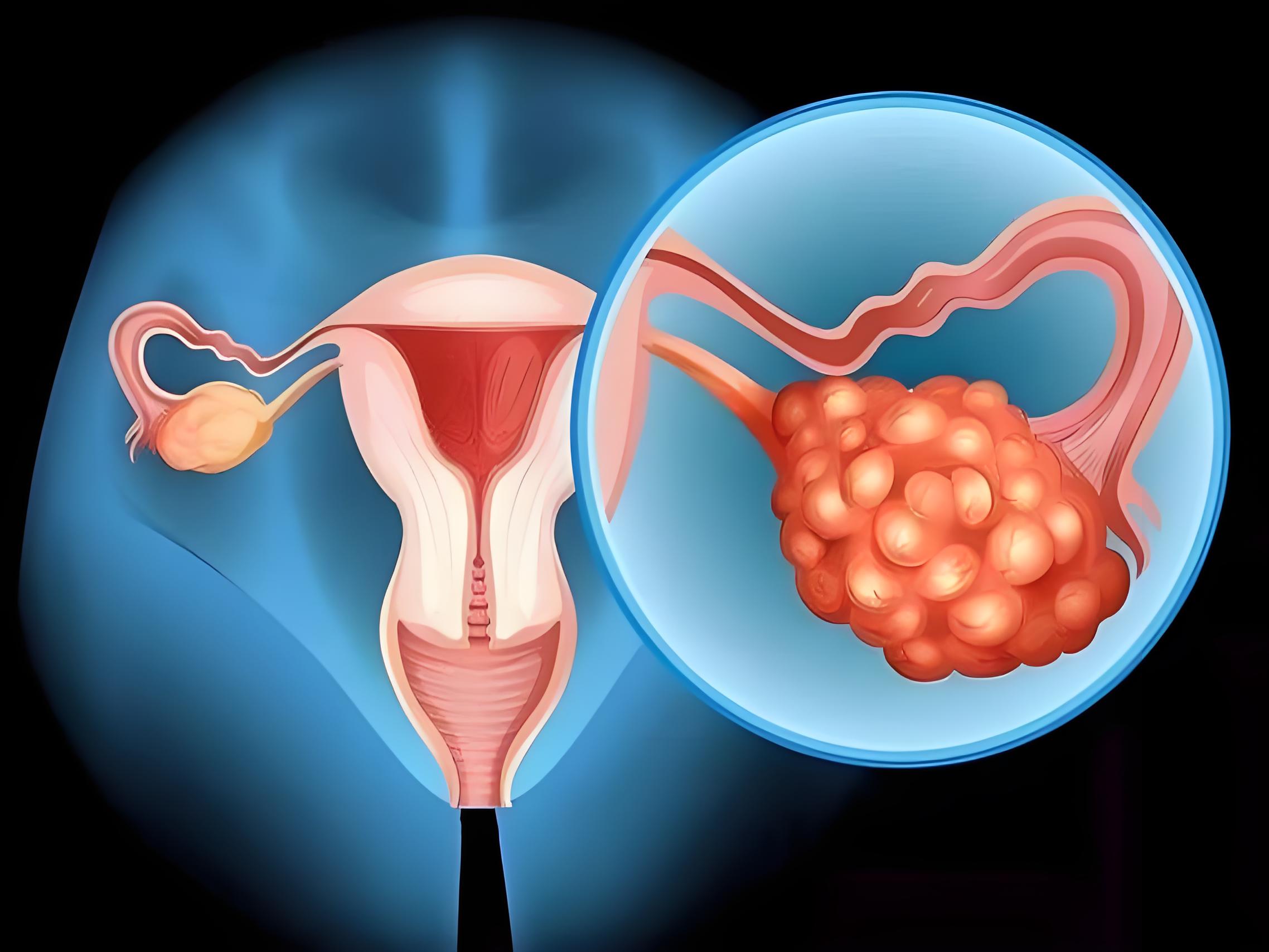
Ovarian Pathology
PCOS ovaries are symmetrically enlarged (2–4× normal size) with a smooth, pearly-white surface. The thickened capsule and subcapsular follicles (≤1.5 cm) reflect chronic anovulation. Theca cell hyperplasia and luteinization surround the follicles, correlating with LH levels and hyperandrogenism.
This translation preserves the technical and clinical nuances of the original text while ensuring clarity for English-speaking readers. Let me know if further refinements are needed! 😊
Share this content:
Leave a Reply